As the Medicaid continuous coverage unwinding progresses, states’ Medicaid renewal data and processes have come under a microscope. Over 4.5 million Medicaid members have lost coverage this year as of August 11, 2023, with 75% having lost coverage due to procedural reasons.1 Ex parte, or automated, renewals is a key strategy to reduce Medicaid churn and to increase efficiency of eligibility staff time. Unfortunately, the rate of ex parte renewals has dropped across the board to 25% during the unwinding2, a reduction from pre-pandemic ex parte rates.
Current unwinding flexibilities that have the potential to be most effective to increase ex parte rates include:
-
Renew eligibility for individuals with no income and no data returned on an ex parte basis. OR
-
Renew eligibility for individuals with income <100% Federal Poverty Line (FPL) and no data returned on an ex parte basis.
These options allow states to complete a Medicaid income determination at renewal without requesting additional information or documentation if:
- The most recent income determination was no earlier than 12 months prior to the beginning of the COVID-19 Public Health Emergency (i.e., March 2019) and was based on verified income at or below 100% FPL or on a verified attestation of zero-dollar income; and
- The state has checked financial data sources in accordance with its verification plan and no information is received.
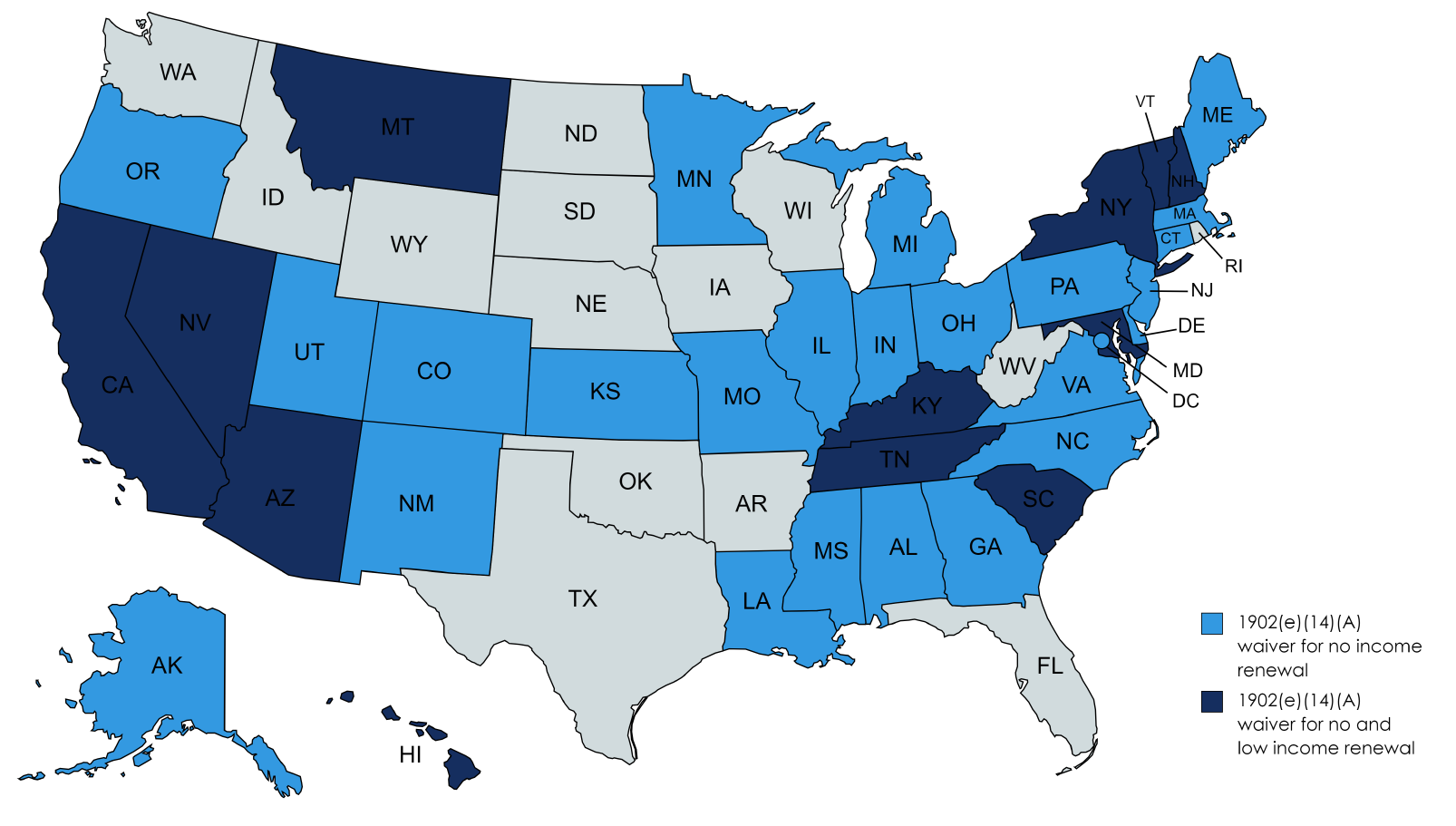
These options can be most effective in increasing ex parte rates for beneficiaries with the lowest income. For example, it may be difficult to verify income for individuals who are self-employed or work at small family-owned businesses, especially in states not using tax data as part of an ex parte determination. Without these options, these beneficiaries would be moved to the active renewal process and would be required to submit additional information or documentation to determine their eligibility, increasing the likelihood of a procedural termination. As of July 27, 2023, 37 states have already elected the 1902(e)(14)(A) option for no income, and twelve of those states have elected to include those with low income.
-
Renew eligibility without regard to an asset test for non-Modified Adjusted Gross Income (MAGI) beneficiaries. This 1902(e)(14)(A) waiver allows states to disregard specific income and asset requirements for older adults and people with disabilities using asset verification systems (AVS). This approach can improve ex parte rates for non-MAGI beneficiaries during unwinding, a group that sees less than a quarter of renewals done via ex parte.6 In addition, this option can make eligibility workers’ time more efficient by reducing any manual asset verification and requiring fewer renewal packets to be reviewed. It can also help the agency save on the cost to run AVS.
States can continue to prioritize policy and process changes to improve ex parte renewal rates after unwinding with the following more permanent flexibilities:
-
Automate renewals for eligible children through Express Lane Eligibility (ELE). Seven states have elected ELE7 to automatically determine if a child can be enrolled or renewed for Medicaid or the Children’s Health Insurance Program (CHIP). Children can be especially vulnerable to losing Medicaid if their parents or caregivers are not eligible for Medicaid or are on a different form of coverage, and they rely on adults in the household to complete a renewal on their behalf. Through ELE, Medicaid and/or CHIP renewal can be determined using information from other programs such as SNAP, TANF, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and Head Start.8 States that have implemented ELE reported reduced churn for children, reduced administrative burden, and cost savings.9
In South Carolina, if there is an active SNAP or TANF case for a child 60 days before their Medicaid renewal, the child is automatically renewed in the eligibility system for 12 months. ELE helped reduce churn in South Carolina, where staff processed over 276,000 renewals, saved 26 minutes per renewal, and saved $1.6 million annually using ELE.
-
Keep low-income workers, seniors, and people with disabilities enrolled by implementing or expanding reasonable compatibility for income and assets. When self-reported income and assets vary from electronic data sources, Medicaid recipients must submit additional documentation to complete their Medicaid renewal. By implementing or expanding a reasonable compatibility standard (RC), beneficiaries who report income and/or assets that vary from what is returned by electronic sources can be automatically verified and renewed if the information reported is within a “reasonable” range. This reasonable compatibility standard is determined by the state and can range between 5-30% and may be different for income and assets. Due to the varied work schedules of low-income workers and the known challenges with producing pay stubs, it is likely that reported income and assets vary from AVS, resulting in manual verifications. Adopting a RC threshold has been identified by CMS as an important strategy for mitigating coverage loss for non-MAGI beneficiaries who have significantly lower ex parte rates compared to MAGI beneficiaries.10 Additional opportunities to improve ex parte rates for non-MAGI beneficiaries are outlined here.
In a state with no reasonable compatibility for assets, when someone reports $800 in a savings account and the AVS reports $900, the eligibility system may not renew automatically and require a more intensive review of paper verification.
-
Automate more renewals with targeted enrollment and renewal strategies using SNAP or TANF. States can pursue temporary unwinding (e)(14)(A) waivers to automatically renew eligibility for certain Medicaid enrollees based on their receipt of SNAP and/or TANF. Many states have 6-month SNAP certification periods or 12-month certification periods with semi-annual reporting11, where income is thoroughly reviewed from the last 30 days, making SNAP a trusted and current data source for Medicaid income verification. Through this integration, when a SNAP recertification is completed, there is potential for the Medicaid renewal period to be pushed forward another 12 months from the SNAP date if SNAP current income meets Medicaid income requirements. Almost all (97%) of people under age 65 receiving SNAP qualify for Medicaid,12 making this streamlining option an opportunity to significantly reduce churn for the MAGI population.
For additional information, please reach out to Miriam Lipschutz, Policy Manager at mlipschutz@bdtrust.org or Jamila McLean, Senior Healthcare Policy Manager at jmclean@bdtrust.org.
This publication was created as part of Benefits Data Trust’s Medicaid Churn Learning Collaborative. Support for this project was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the Foundation.
