Four years ago, Benefits Data Trust (BDT) teamed up with one of our longtime partners in healthcare to produce deeper evidence that food indeed is medicine. Together with the UPMC Center for High-Value Health Care, we set our sights on studying one specific population: people eligible for both Medicare and Medicaid. These individuals are unique among low-income groups because they face complicated health conditions and higher-than-average health care costs. For example, consider a grandmother with low income who lives with multiple chronic conditions such as diabetes, kidney disease, congestive heart failure, arthritis, and depression.
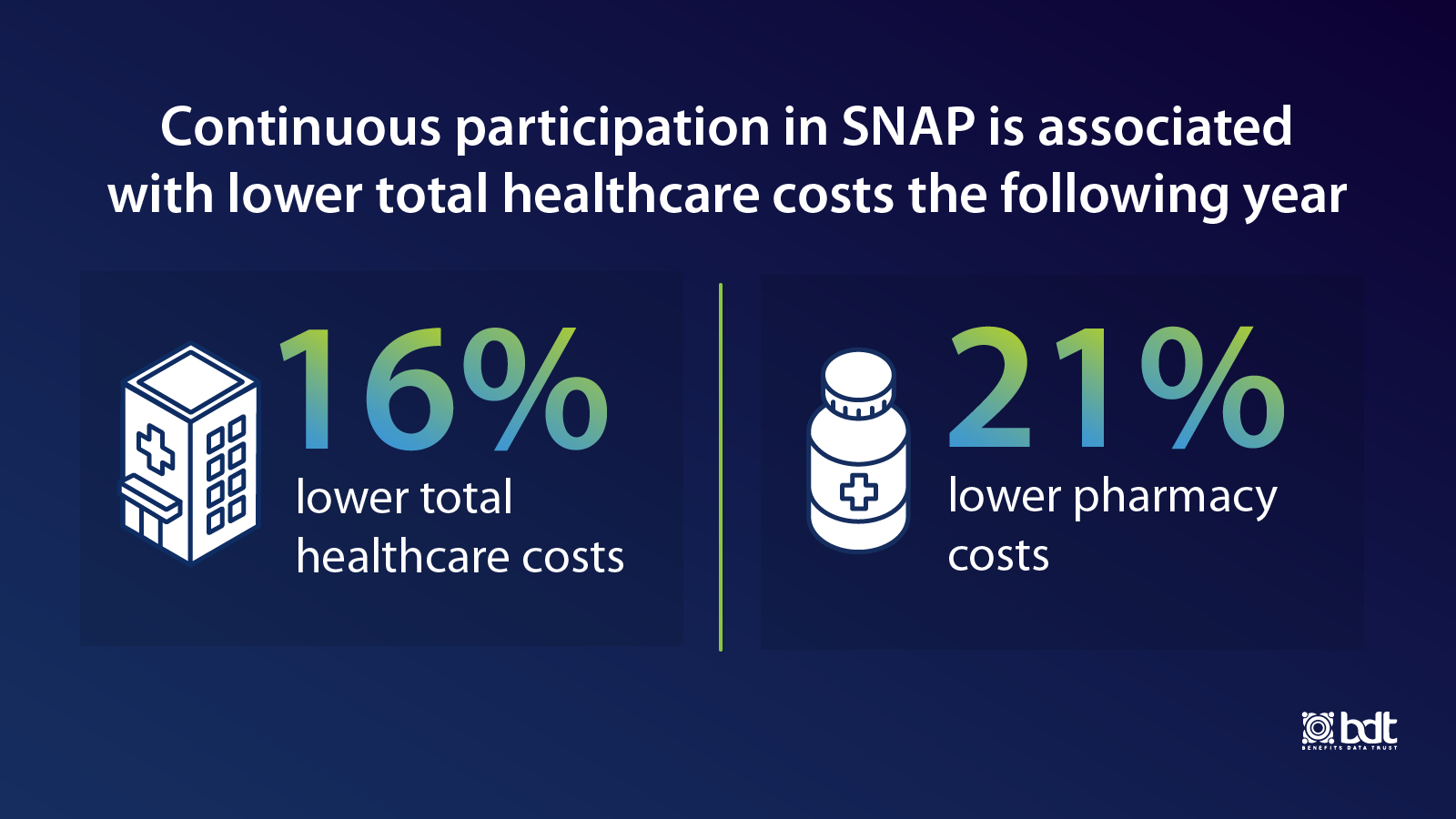
Our research, funded by the Robert Wood Johnson Foundation’s Systems for Action program, was published recently in the peer-reviewed journal NEJM Catalyst Innovations in Care Delivery. We found that one year of continuous participation in the Supplemental Nutrition Assistance Program (SNAP) is associated with lower healthcare costs the following year.
We compared two groups with similar demographic characteristics – where one group was enrolled in SNAP and the other was not – and the data showed that the people participating in SNAP incurred health care costs that were 16 percent lower and pharmacy costs that were 21 percent lower. These lower costs were experienced within the first year after 12 months of SNAP enrollment.
Our study, which involved 661 SNAP participants and 1320 non-participants enrolled in UPMC Health Plan’s Community Health Choices plan for dual-eligible individuals, adds to a significant body of research that has strengthened consensus that food and nutrition security is linked with better health outcomes and reduced health costs.
Previously, in Maryland, BDT’s data helped demonstrate that SNAP participation among individuals eligible for both Medicare and Medicaid was associated with $2,100 in average per-person healthcare savings. And in North Carolina, our data shows that SNAP enrollment for older adults is associated with an average Medicaid cost-savings of $2,360 a year per person, as well as fewer hospital and long-term care admissions and emergency room visits.
Yet how best to deliver food and nutrition security programs that are cost-effective – and scalable – is less clear.
Collaborations between the healthcare system and non-profits offer a promising solution, as demonstrated by the ongoing partnership between BDT and UPMC Health Plan, which have worked together since 2018 to connect eligible insurance plan members to food assistance benefits like SNAP.
Through our partnership, UPMC Health Plan recognized the opportunity to support food and nutrition security among tens of thousands of members of its Community HealthChoices plan by offering public benefits screening and application assistance. To date, BDT has submitted more than 10,000 applications for SNAP and other public benefit programs on behalf of UPMC Health Plan members.
Key Questions this Study Raises
While our study affirms previous findings that SNAP enrollment is linked to lower healthcare costs, we identified notable differences that raise compelling questions and invite further research:
-
Types of Costs Reduced: Other studies have found major reductions in emergency department (ED) or inpatient care use for those enrolled in SNAP, yet ours showed that pharmacy costs drove the overall cost reduction. One reason may be that SNAP helps stabilize people’s food intake, potentially requiring fewer doses of as-needed medications that treat flareups in illnesses like congestive heart failure or diabetes. Another contributing factor may have been timing: this study included data from 2018 through 2021, a period when ED and inpatient care use were likely impacted for both the study and comparison groups by the COVID-19 pandemic’s effect on healthcare use patterns.
Further study is needed into the relationship among SNAP enrollment, specific cost reductions, and the patient experience. Greater understanding could unlock key refinements in how healthcare organizations design their food and nutrition security programs.
-
Duration of SNAP Enrollment: We used a stricter definition of SNAP participation (12 months of continuous enrollment) than other studies have (e.g., enrollment of any length within the previous 12 months.) Further research is necessary to understand the links among health outcomes, costs, and the duration of SNAP enrollment, particularly the effects to someone’s health if they lose SNAP coverage or experience SNAP churn.
To learn more about our healthcare initiatives and how we can work with you, contact Ashley Humienny at ahumienny@bdtrust.org
For more information about data sharing to support outreach and evaluation, check out BDT's Data Sharing Playbook.
